Remote Patient Monitoring (RPM) has grown fast in the past few years. Because of this rise, CMS updates the billing rules every year to make them clearer and easier to follow. These changes help clinics bill the right way and protect patient care quality.
The 2026 RPM CPT code update brings new rules, fresh clarifications, and a few changes that clinics should know about. Even small updates can impact billing, revenue, and compliance. If your team works with Medicare patients, staying updated now will help you avoid mistakes later.
Studies show that remote monitoring can lower hospital visits by up to 25% for hypertension patients (Source: American Heart Association). With clear billing rules for 2026, clinics can continue this care without confusion.
This guide explains what’s new, what stayed the same, and how to prepare for the 2026 RPM CPT code changes.
If you want a system that stays updated with every CPT change, CandiHealth helps clinics set up RPM, manage patient alerts, and stay compliant without adding more work to your staff.
What’s New in the 2026 Remote Patient Monitoring CPT Codes?
CMS has clarified how many days count toward RPM, what qualifies as interactive time, how devices must transmit data, and what documentation clinics need to support each billed code. Some codes may also include adjusted reimbursement rates for 2026.
These changes help clinics avoid errors and support cleaner, faster billing. Below are the sections that explain every part in detail.
Overview of 2026 RPM Code Changes (Quick Table)
Here is a table reflecting the new codes plus existing ones, with what changed for 2026 (or will apply effective January 1, 2026).
Note: Always verify with the final rule from Centers for Medicare & Medicaid Services (CMS).
| CPT Code | What Changed in 2026 | Old Rule | New Rule | Why It Matters |
| 99453 | Remains for initial setup & education; no new alternate code yet | One-time setup service | No change to core descriptor | Stability in your setup billing |
| 99454 | Now applies to 16-30 days of data in 30-day period; new shorter-duration code added | Required 16+ days of data for device supply | Splits: 99454 (16-30 days) and new code 99445 (2-15 days) for device supply | Captures patients needing shorter monitoring periods (Medical Office Force) |
| 99445 (NEW) | New code for device supply/data transmission for 2-15 measurement days in a 30-day period | Did not exist previously | Bill for 2-15 days of data rather than waiting for 16 days | Opens RPM to more patients/shorter episodes (rimidi.com) |
| 99457 | Remains first 20 minutes of treatment management; code remains valid | First 20 minutes month requirement | No alternate time code added here; however new shorter-time code introduced | Keeps core time-based billing stable |
| 99470 (NEW) | New code for “first 10 minutes” of RPM treatment management (10-19 minutes) | No code for <20 minutes before | Bill for 10-19 minutes using 99470; 99457 remains for 20+ | Captures shorter, meaningful patient interactions (Medical Office Force) |
| 99458 | Additional 20-minute increments remain valid for 20+ extra minutes | Additional 20 minutes increments | No change in structure, but must coordinate with new 99470 if shorter time used | Ensures clinics capture longer interactions without missing shorter ones |
Key notes:
- The two new codes (99445 and 99470) are not additive to the existing codes in the same category. For instance, you cannot bill 99445 and 99454 for the same 30-day period.
- The existing codes remain valid. The new ones simply provide more flexibility.
- The “16-day rule” for the 99454 code remains unchanged – if you use that code, the patient still needs 16 measurement days (unless you bill 99445 for 2-15 days). Medical Office Force
- Documentation and coding workflows will need updates to handle the new codes.
Updated Billing Rules for 2026
Here are the updated billing rules, with the new codes incorporated and wording adjusted for accuracy:
Measurement-Days Rules
- For code 99445 (NEW): Billable when you supply a device and collect data for 2-15 days in a 30-day period.
- For code 99454: Billable when you supply a device and collect data for 16-30 days in a 30-day period.
- Only one of these codes may be billed per device/patient per 30-day period (you choose based on measurement-days).
- Devices must still automatically transmit data (not manually entered) and must be FDA-cleared.
Device Requirements
- Devices must be FDA-cleared and support automatic data transmission (not just manual entry).
- Each patient must have their own device or comply with CMS guidance for shared use.
- Whether billing 99445 or 99454, the device supply within the 30-day window must be documented.
Time/Interactive Communication Rules
- For code 99470 (NEW): Billable when you spend 10-19 minutes of treatment management time in a calendar month, including at least one live interactive communication (video or phone) with the patient or caregiver.
- For code 99457: Remains billable for 20+ minutes of treatment management time in a calendar month including one live interactive communication.
- For code 99458: Use for each additional 20 minutes beyond the first 20 minutes (when 99457 applies) in a single month.
- Live interactive communication is required (phone or video) for both 99470 and 99457 codes. Documentation must include start time, end time, summary, clinician involved.
Documentation and Coding Workflows
- Decide which measurement-days code (99445 vs 99454) applies based on data days transmitted.
- Track cumulative clinical staff/qualified practitioner time each calendar month to determine whether 99470 or 99457 applies.
- If you achieve 20+ minutes, use 99457 rather than 99470. 99470 only when the time is 10-19 minutes.
- Maintain documentation: device activation date, number of days of data transmission, interactive communication details, clinical decisions/alerts, device inventory.
- Ensure that RPM services do not duplicate billing with other programs (eg. Remote Therapeutic Monitoring (RTM) if same condition), unless CMS allows.
Revenue & Compliance Implications
- The new codes allow billing for shorter monitoring episodes (2-15 days) and shorter clinical interactions (10-19 minutes).
- This change can increase revenue opportunities because clinics no longer must meet longer thresholds before billing.
- Compliance remains key: billing the wrong code (e.g., using 99454 for 10 days of data) may lead to claim denials or audits.
New Clarifications From CMS for RPM (2026 Update)
CMS has shared clearer rules for RPM in 2026. These updates help clinics bill the right code, use the right time rule, and avoid confusion with the new measurement-days and time-based codes. The goal is simple: accurate reporting and clean claims.
Here are the key clarifications for 2026:
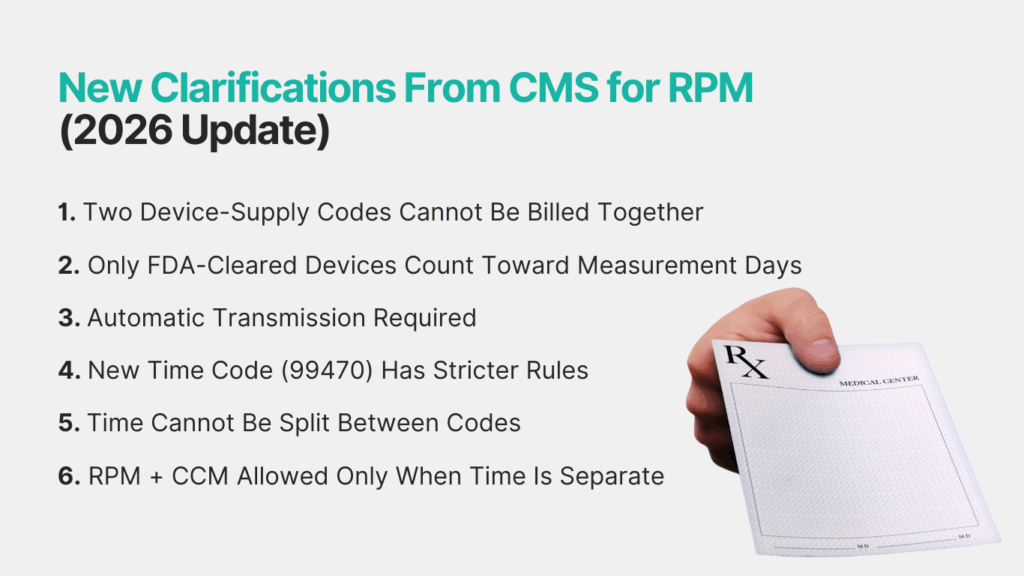
1. Two Device-Supply Codes Cannot Be Billed Together
CMS confirmed that 99445 (2–15 days) and 99454 (16–30 days) cannot be billed in the same 30-day period. You must choose one based on the patient’s measurement days.
Simple rule:
2–15 days → 99445
16–30 days → 99454
2. Only FDA-Cleared Devices Count Toward Measurement Days
CMS repeated that only medical-grade, FDA-cleared devices qualify. Apps, manual entry tools, and wearables without FDA clearance do not count for 99445 or 99454. This prevents misuse of low-accuracy devices.
3. Automatic Transmission Required
A counted day must have:
- A real reading
- Sent automatically from the device
- Stored in the practice system
Manual entry does not count as a measurement day.
4. New Time Code (99470) Has Stricter Rules
The new 2026 code 99470 allows billing for 10–19 minutes of RPM management time.
CMS clarified that these minutes must include:
- At least one live interaction (phone or video)
- Time must be measurable and documented
- Non-live messages do NOT count
If the clinician reaches 20 minutes, clinics must bill 99457, not 99470.
5. Time Cannot Be Split Between Codes
CMS explained that:
- If a clinic reaches 10–19 minutes → bill 99470
- If it reaches 20+ → bill 99457
- You cannot combine both in the same month for the same patient
Time accumulates within the calendar month.
6. RPM + CCM Allowed Only When Time Is Separate
CMS restated that:
- RPM time and CCM time must be separate
- You cannot count the same minutes for both services
- Both can be billed if documentation supports separate efforts
This helps clinics increase revenue while staying compliant.
2026 Reimbursement Rates
CMS has not released the final 2026 national payment rates yet. But CMS has shared how the new codes will be paid and how each code fits into the 2026 Physician Fee Schedule. The update shows a clear structure: the new codes (99445 and 99470) will be paid as stand-alone services with their own RVUs (Relative Value Units).
Here’s what CMS has confirmed so far:
How CMS Will Pay RPM Codes in 2026
CMS uses three things when deciding the final payment:
- Work RVUs
- Practice expense value
- Geographic adjustment
This means the final amount clinics receive can vary by state. But the billing structure for 2026 is clear:
Expected Payment Structure
Below is a clean table showing how each code category will be paid. Note: This table explains the structure, not exact dollar amounts, until CMS publishes the final rates.
| CPT Code | What It Covers | How CMS Will Pay It in 2026 | Notes |
| 99453 | Device setup & patient onboarding | Paid once per episode per patient | No change |
| 99445 (NEW) | 2–15 days of device supply & transmission | Paid at a lower rate than 99454 (because fewer days) | New code for shorter monitoring |
| 99454 | 16–30 days of device supply & transmission | Paid as the primary device-supply code | Cannot bill with 99445 |
| 99470 (NEW) | 10–19 minutes of RPM treatment management | Paid at a lower RVU than 99457 | First 10-minute management code |
| 99457 | First 20+ minutes of management time | Paid at higher RVU than 99470 | Must include 1 live interaction |
| 99458 | Each extra 20 minutes | Paid as an add-on code | Cannot be billed with 99470 |
What Clinics Should Expect
While exact values will come later, CMS will continue the same pattern:
Higher payments for codes tied to more time or more data
- 99454 > 99445
- 99457 > 99470
Two new codes will expand billable opportunities
- Shorter monitoring episodes
- Shorter interaction time
Rates may adjust slightly for inflation or budget neutrality
CMS typically updates RVUs every year based on national spending targets.
Final Thoughts
The 2026 RPM CPT code changes give clinics more flexibility and clearer rules. With the two new codes—99445 for short monitoring periods and 99470 for shorter clinical time—more patients can be covered, and more of your team’s work can be billed the right way. These updates also set stronger standards for device use, documentation, and live interactions, which helps clinics stay compliant and avoid billing mistakes.
For clinics that treat large numbers of hypertension or chronic care patients, these changes can improve both outcomes and revenue. The key is having the right tools to track device days, manage clinical time, and follow CMS rules without adding extra work to your staff.
CandiHealth helps clinics stay ready for 2026 with:
- Pre-configured cellular BP devices
- Automatic measurement-day tracking
- Clear time logging for 99470, 99457, and 99458
- Real-time alerts
- Easy onboarding and support
- Built-in billing and compliance workflows
If you want an RPM program that stays compliant with every CMS update, and works right out of the box, CandiHealth is here to support your clinic.
Start your RPM program with CandiHealth today and get a setup designed for the new 2026 billing rules.
FAQs: 2026 Remote Patient Monitoring CPT Codes
What are the new RPM codes for 2026?
CMS introduced two new codes: 99445 for 2–15 days of device data and 99470 for 10–19 minutes of RPM management time. These codes help clinics bill shorter monitoring periods and shorter clinical interactions.
2. Can I bill 99445 and 99454 in the same month?
No. You must choose one.
- 99445 → 2–15 days
- 99454 → 16–30 days
CMS does not allow both codes in the same 30-day cycle for the same patient.
3. Does manual entry count toward measurement days?
No. CMS requires readings to be auto-transmitted from an FDA-cleared device. Manual typing, apps, or consumer wearables do not count toward 99445 or 99454.
4. What counts as “interactive time” for 99470 and 99457?
Only a live phone or video call counts. Text, portal messages, and automated reminders do not qualify. At least one live interaction is required for both 99470 and 99457.
5. Can I bill RPM and CCM together?
Yes, but you must separate the time. The minutes you use for RPM cannot be counted again for CCM. Both can be billed when documentation is clear.
6. Can I bill RPM and RTM for the same patient?
No. CMS does not allow RPM and RTM to be billed for the same condition in the same month. You must pick one based on the clinical need.
7. What device qualifies for RPM in 2026?
Only FDA-cleared, medical-grade, automatically transmitting devices qualify. Consumer wearables or manual BP cuffs are not allowed for billing measurement days.
8. Do I need 16 days of data to bill RPM in 2026?
Only if you are billing 99454. For shorter monitoring episodes (2–15 days), use 99445.
9. What happens if the patient only sends readings for 8–10 days?
You can bill 99445, as long as data was auto-transmitted and device rules were followed.
10. How can clinics stay compliant with the 2026 changes?
Use FDA-cleared devices, track measurement days automatically, document start dates and clinical minutes, and ensure at least one live interaction each month. Using a platform like CandiHealth makes this easy.