Remote patient monitoring (RPM) has become a key part of care for seniors and patients with chronic conditions. But for many years, clinics struggled with the business side of RPM. The billing rules were strict, and even small gaps, like a patient missing a few readings, could stop a clinic from getting paid. At the same time, Medicare’s conversion factor kept dropping, which lowered payments even further.
Now, CMS has approved new RPM updates for 2026. These changes fix many of the old barriers. Two new CPT codes will now cover shorter monitoring days and partial-month staff time. CMS has also increased the conversion factor for the first time in years. Together, these updates make RPM revenue easier and help more patients qualify for monitoring.
In this blog, we explain what changed, why these updates matter, and how clinics can prepare to earn more from RPM in 2026.
How New CMS Rules Make Generating ROI on RPM Even Easier
The new CMS rules make RPM ROI easier by paying for more types of patient activity. Shorter monitoring days and partial-month staff time will now be reimbursed. CMS also increased the conversion factor, which raises overall payment rates. These updates help clinics bill more often, support more patients, and earn steady monthly revenue.
To explain this clearly, the next sections will cover:
- Why clinics struggled with RPM revenue before
- What changed in the 2026 CMS final rule
- How the two new CPT codes help your RPM program
- How the higher conversion factor boosts payment
- A simple example showing real revenue gains
- Steps clinics should take before January 2026
- Why the right RPM partner matters for compliance and cost
Why RPM ROI Was Hard Before 2026
Many clinics liked the idea of remote patient monitoring, but earning steady revenue from it was not always easy. Several rules made it harder for clinics to bill even when real work was done. Here are the main reasons:
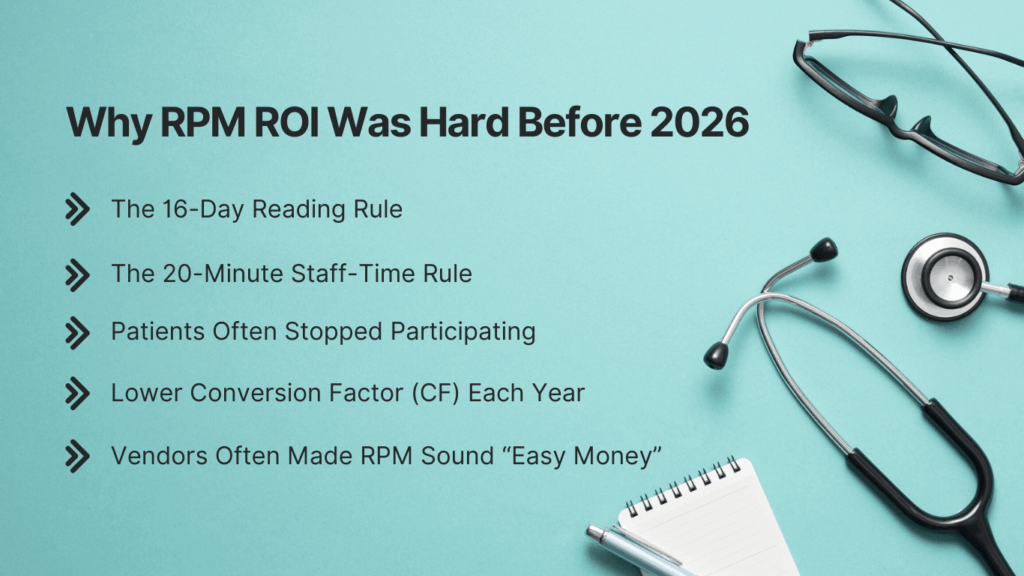
1. The 16-Day Reading Rule
To bill the device-supply code (99454), patients had to send at least 16 days of readings in one month. If a patient missed a few days, the clinic could not bill — even if the readings they did send were helpful.
2. The 20-Minute Staff-Time Rule
To bill the management code (99457), staff had to document 20 minutes of support each month. But some patients only needed 10–15 minutes. That work was real, but it was not billable.
3. Patients Often Stopped Participating
Many patients forgot to take readings daily. This led to skipped days → lost billing → lost revenue.
4. Lower Conversion Factor (CF) Each Year
For several years, Medicare’s conversion factor kept dropping.
A lower CF means:
- Clinics got paid less for the same work.
- RPM programs became harder to maintain without strong volume.
Vendors Often Made RPM Sound “Easy Money”
Some clinics were told RPM would bring fast revenue, but the older CMS rules made it hard to:
- Meet all requirements
- Keep patients engaged
- Bill every eligible month
These challenges created a gap between clinical value and financial return. The 2026 CMS updates fix many of these issues and make RPM ROI more stable and predictable.
What Changed in the 2026 CMS Physician Fee Schedule?
CMS has made several updates for 2026 that remove old RPM barriers and open new billing opportunities. These changes help clinics bill more often, include more patients, and get paid for work that was not reimbursed before.
Below are the biggest updates you need to know.
1. New CPT Code 99XX5 (2–15 Days of Readings)
This new code pays clinics for 2 to 15 days of patient readings in a 30-day cycle. Before 2026, only patients with 16 days of readings qualified for payment. Now, shorter monitoring periods are fully billable. This helps:
- Patients who take fewer readings
- Medication adjustment cases
- Post-surgery patients
- Hypertension patients who are stable
- Rural patients with slow or inconsistent internet
2. New CPT Code 99XX4 (10–20 Minutes of Staff Time)
This code pays for 10 to 20 minutes of RPM treatment management. Before 2026, clinics only got paid if they reached 20+ minutes. Now, shorter but meaningful work is reimbursed, such as quick check-ins, medication reminders, reviewing fewer readings and guiding patients who only need light support.
3. Full Payment Maintained for 99457 and 99458
CMS did not reduce payment for the existing 20-minute codes. This means:
- Full value for 20+ minute encounters stays the same
- Clinics don’t lose money if they deliver longer care
- Partial-month and full-month work are now paid fairly
4. Higher Conversion Factor (CF) for 2026
For the first time in years, CMS increased the conversion factor.
- $33.40 for non-APM clinicians
- $33.57 for APM participants
This raises reimbursement across most RPM and CCM time-based codes. Even a small CF increase boosts annual earnings for busy RPM programs.
5. Hospital Outpatient Data Included in Rate Setting
CMS will now use hospital outpatient department (HOPD) cost data when updating certain values. This gives RPM a more realistic cost basis because:
- Monitoring takes real resources
- Staff time and device costs are higher today
- Data more closely reflects real practice expenses
This signals CMS sees RPM as an essential care service, not an optional add-on.
Summary Table: What Changed from 2025 to 2026
| Area | 2025 Rules | 2026 Rules |
| Device Readings | Must reach 16 days | 2–15 days now billable (99445) |
| Staff Time | Must reach 20 minutes | 10–20 minutes now billable (99470) |
| Conversion Factor | $32.35 | $33.40 / $33.57 |
| Billing Flexibility | Low | High |
| Short-Term Monitoring | Not paid | Fully reimbursed |
| Rural Patient Support | Hard to bill | Much easier |
How These New Rules Improve RPM ROI for Clinics
The 2026 CMS updates make RPM easier to run and easier to bill. Clinics can now earn revenue from more types of patient activity, even when readings or staff time do not reach the old limits. This creates a more stable and predictable RPM program.
Here are the main ways these rules improve ROI.
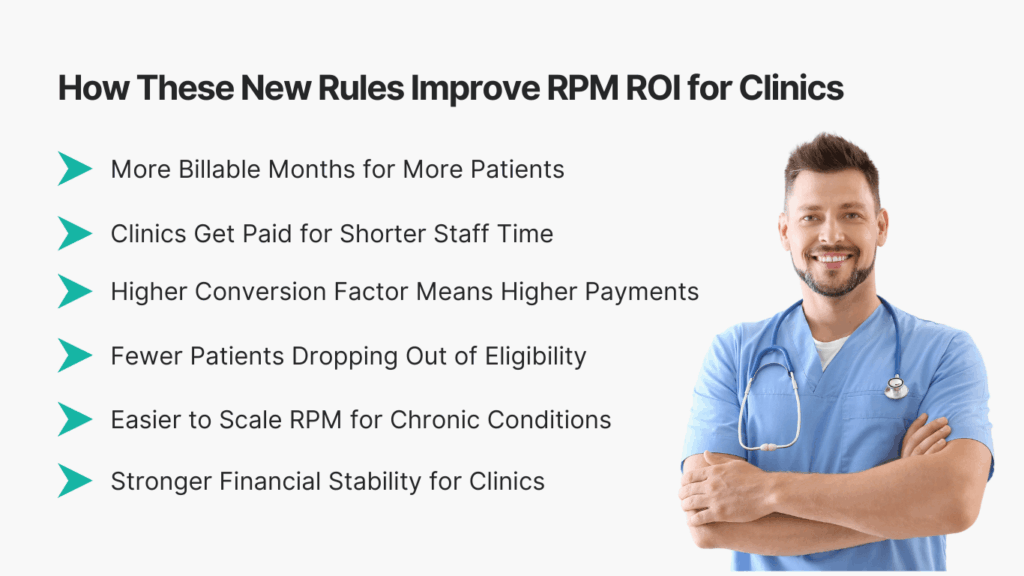
1. More Billable Months for More Patients
In the past, many patients missed the 16-day rule. Now, with the new 99445 code for 2–15 days:
- Light-monitoring patients can be billed
- Rural patients are less likely to “lose the month”
- Stable hypertension patients still count
- Post-surgery and medication-change patients qualify
More patients meeting billing rules = more monthly revenue.
2. Clinics Get Paid for Shorter Staff Time
The new 99470 code pays for 10–20 minutes of work. This means clinics get reimbursed for:
- Quick follow-ups
- Short health coaching
- Reviewing fewer readings
- Medication reminders
- Mini check-ins
Before 2026, this time was not paid at all. Now, every real action has a path to reimbursement.
3. Higher Conversion Factor Means Higher Payments
Because the CF is rising in 2026:
- RPM payments increase
- Time-based codes become more valuable
- Programs that were “just breaking even” now show profit
Even small CF increases add up when clinics manage large patient groups.
4. Fewer Patients Dropping Out of Eligibility
Under old rules, one missed reading could ruin the entire billing month. Now, even partial activity is billable. This means:
- Less pressure on daily reminders
- Less staff time wasted on chasing readings
- Better patient experience
- Higher compliance
Higher compliance = lower operational costs + higher monthly billing.
5. Easier to Scale RPM for Chronic Conditions
Conditions like high blood pressure, diabetes, COPD, and heart failure often require small but steady monitoring. With new CPT flexibility:
- Mild cases can now be enrolled
- Patients with stable readings still count
- Shorter monitoring programs now make financial sense
This creates a larger pool of eligible patients.
6. Stronger Financial Stability for Clinics
The updates shift RPM from a “high-effort, low-return” service into a more balanced program. Clinics gain:
- Steady recurring revenue
- More billable encounters
- Clearer documentation rules
- Easier workflows
- Better staff efficiency
How Clinics Can Prepare for the 2026 RPM Rules
The new CMS rules open the door for better RPM revenue, but clinics must be ready before January. A few small steps can make the transition smooth and help your team bill correctly from day one. Here is a simple checklist to follow.
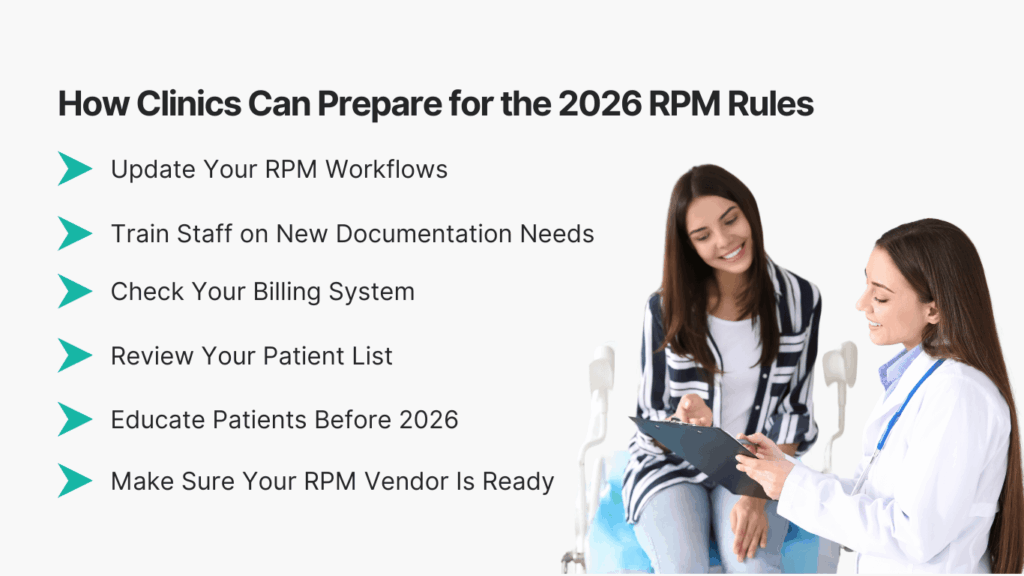
1. Update Your RPM Workflows
Make sure your team knows the new rules for:
- 2–15 day readings (CPT 99445)
- 10–20 minute staff time (CPT 99470)
- 16+ day and 20+ minute codes that stay the same
Clear workflows help prevent missed billing months.
2. Train Staff on New Documentation Needs
Your team should know how to log reading days, track staff time, record short interactions and note missed readings correctly. Good notes make billing faster and cleaner.
3. Check Your Billing System
Make sure your billing software supports the new CPT codes:
- 99445 (2–15 days)
- 99470 (10–20 minutes)
Add them now so your team does not waste time in January.
4. Review Your Patient List
Look for patients who:
- Only send a few readings each mont
- Only need short check-ins
- Have stable blood pressure or weight
- Live in rural areas with low internet
These patients can now be enrolled or re-enrolled under the new rules.
5. Educate Patients Before 2026
Tell patients:
- How many days of readings they need
- How the process works
- Why their readings matter
- What has changed for 2026
This boosts compliance and helps you bill every month.
6. Make Sure Your RPM Vendor Is Ready
Your vendor should support:
- Shorter monitoring periods
- Cellular devices for easy transmissions
- Fast onboarding
- Alert management
- Automatic time tracking
- Easy dashboards for staff
If your vendor is slow to adapt, you may lose revenue.
Final Thoughts
The 2026 CMS rules are a major step forward for remote patient monitoring. By adding new CPT codes and raising the conversion factor, CMS has fixed many of the problems that made RPM hard to bill in the past. Clinics can now earn from shorter monitoring days, shorter staff-time work, and patients who only need light monthly support. This makes RPM more flexible, more reliable, and easier to run.
For clinics already using RPM, these updates can quickly improve revenue. For clinics that paused or never started RPM, 2026 is the best time to begin. With the right tools and clear workflows, RPM can support better patient care and create steady monthly income.
CandiHealth is built to help clinics make the most of these changes. Our cellular devices, simple dashboards, automatic time tracking, and $10 flat-fee model remove the stress that often comes with RPM. We help your team follow CMS rules, reduce missed readings, and bill with confidence.
Want to see how your clinic can earn more under the 2026 rules? Book a quick 10-minute demo with CandiHealth and get started.
Frequently Asked Questions (FAQs)
1. What are the new RPM CPT codes for 2026?
CMS added two new codes for 2026:
- 99445 for 2–15 days of patient readings
- 99470 for 10–20 minutes of staff time
These codes make it easier for clinics to bill for shorter monitoring periods and short check-ins.
2. Do clinics still need 16 days of readings to bill RPM?
Not always. The old 16-day rule still applies for 99454, but clinics can now bill 99445 for patients who only send 2–15 days of readings. This helps clinics support more patients and bill more consistently.
3. Can clinics bill for less than 20 minutes of staff time?
Yes. The new code 99470 allows billing for 10–20 minutes of RPM management. This means shorter follow-ups, quick coaching, or brief medication checks are now reimbursed.
4. How does the 2026 conversion factor increase affect RPM revenue?
The conversion factor is rising to $33.40 (non-APM) and $33.57 (APM). This increase boosts payment for all time-based RPM codes, leading to higher monthly revenue, especially for clinics monitoring large patient groups.