Remote Patient Monitoring (RPM) has become one of the fastest-growing care models in the U.S. healthcare system. With Medicare spending on RPM rising from $6.8 million in 2019 to nearly $194 million in 2023, both clinics and payers are now investing heavily in partnerships that improve patient outcomes and reduce costs.
But while the opportunity is clear, the process isn’t always simple. Whether you’re an RPM vendor, healthcare startup, or technology provider, knowing how to partner effectively with clinics or payers is what determines long-term success.
This guide breaks down exactly how to partner with clinics or payers for RPM, the models available, compliance essentials, and actionable steps to help you scale your RPM business confidently.
If you’re exploring partnership opportunities, CandiHealth helps simplify the process with plug-and-play RPM programs, cellular devices, and a flat-fee model for predictable costs.
How to Partner with Clinics or Payers for RPM?
To partner with clinics or payers for Remote Patient Monitoring (RPM), you need to build trust through compliance, clear ROI, and seamless integration. The process involves identifying the right partner, presenting measurable outcomes, and setting up shared workflows that make patient monitoring effortless for both sides. In simple terms:
- Clinics look for RPM partners who can improve care quality, automate follow-ups, and boost reimbursement with minimal effort.
- Payers seek proven RPM models that reduce hospital readmissions and long-term healthcare costs.
Successful RPM partnerships follow two main routes:
- Clinic Partnerships work directly with healthcare providers or group practices to implement RPM for their patient base.
- Payer Partnerships collaborate with insurance companies to scale RPM across their network and improve population health outcomes.
Each model has its own benefits, compliance needs, and onboarding steps, which we’ll break down next.
How to Partner with Clinics for RPM?
Partnering with clinics is often the fastest and most direct way to launch or scale your RPM program. Clinics already have the patient base, trust, and reimbursement structure, what they need is a reliable, compliant, and easy-to-use solution. Here’s a step-by-step process to build strong RPM partnerships with clinics.
- Identify the right clinics
- Present a clear value proposition
- Set up a demo and ROI discussion
- Simplify compliance and onboarding
- Create a shared workflow
- Provide ongoing support and reporting

Look at the details below.
Step 1: Identify the Right Clinics
Start with clinics that treat chronic conditions like hypertension, diabetes, or heart disease, as they qualify for Medicare-covered RPM services.
Look for:
- Primary care practices (especially independent ones).
- Cardiology and nephrology clinics.
- Rural or underserved clinics seeking extra support and reimbursement.
Use data tools like Medicare provider databases or networking platforms (e.g., Apollo.io, LinkedIn, or medical conferences) to find practices that match your goals.
Step 2: Present a Clear Value Proposition
Clinics are busy, they won’t respond to generic pitches. Focus on showing ROI and reduced workload. Your message should highlight:
- How RPM increases patient engagement and retention.
- The financial benefit (average $120 per patient/month in Medicare reimbursement).
- How your platform handles logistics like enrollment, device shipping, and monitoring.
Example: “If your clinic enrolls 50 hypertension patients, you can generate around $6,000 per month in new revenue while improving patient outcomes.”
Step 3: Set Up a Demo and ROI Discussion
Before discussing pricing, schedule a live demo with the clinic’s administrator or physician. Show them:
- How the platform works (data flow, alerts, dashboards).
- The patient experience (device setup, readings, alerts).
- Real-world examples of improved outcomes.
Use ROI calculators or case studies (like those provided by CandiHealth) to visualize the financial and clinical value.
Step 4: Simplify Compliance and Onboarding
Compliance is often what holds clinics back from launching RPM. Make it easy by providing:
- HIPAA-compliant documentation and Business Associate Agreements (BAA).
- Staff training kits on CPT codes (99453-99458).
- Patient consent templates for easy enrollment.
CandiHealth, for example, supports clinics with pre-configured cellular devices and automated alerts, reducing administrative load.
Step 5: Create a Shared Workflow
To ensure long-term success, define how responsibilities will be shared between your team and the clinic. A simple structure looks like this:
| Task | Clinic’s Role | RPM Partner’s Role |
| Patient enrollment | Verify eligibility & consent | Provide enrollment tools |
| Device setup | Educate patient | Ship and configure devices |
| Monitoring | Review flagged alerts | Maintain data and dashboards |
| Billing | Submit CPT claims | Support documentation & reporting |
Step 6: Provide Ongoing Support and Reporting
After launch, keep the partnership strong by:
- Offering monthly performance reports (enrolled patients, readings, billing).]
- Conducting quarterly reviews to discuss growth opportunities.
- Providing 24/7 technical support for staff and patients.
Clinics appreciate consistency and when they see measurable improvements in outcomes, referrals naturally follow.
How to Partner with Payers for RPM?
Partnering with payers takes your RPM business from small-scale clinic collaboration to large-scale, system-wide impact. Unlike clinics that focus on individual patient care, payers care about outcomes at scale, lowering costs, reducing hospital readmissions, and improving population health.
To form successful payer partnerships, you need to position your RPM program as a cost-saving, compliance-ready, and data-driven solution. Below is a step-by-step guide on how to partner with payers of RPM.
- Understand payer priorities
- Build a data-backed business case
- Offer flexible partnership models
- Demonstrate compliance and integration readiness
- Engage through pilot programs
- Provide Transparent Reporting and Support
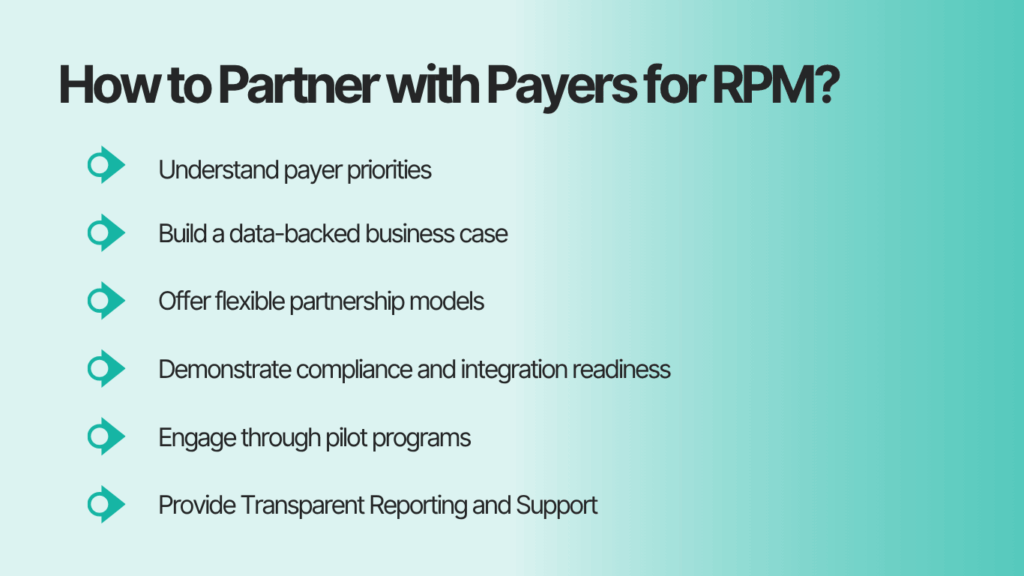
Here is the detailed description of each.
Step 1: Understand Payer Priorities
Before approaching any insurer, research what matters most to them. Most payers focus on:
- Reducing hospital readmissions and ER visits.
- Managing chronic conditions (hypertension, diabetes, COPD).
- Improving HEDIS and STAR ratings for quality measures.
Start by targeting Medicare Advantage and regional insurance networks that already fund RPM or value-based care initiatives.
Step 2: Build a Data-Backed Business Case
Payers want proof, not promises. Present your partnership proposal with measurable evidence.
Include:
- Clinical outcome data (e.g., reduced systolic BP by 8 mmHg in 3 months).
- Cost savings (e.g., 20% reduction in readmissions).
- Patient engagement metrics (e.g., 85% device usage compliance).
If you’re early-stage, use published studies and CMS case data to demonstrate industry-backed results. Example: According to the American Heart Association, effective home monitoring can reduce hospitalizations by 25% for hypertensive patients.
Step 3: Offer Flexible Partnership Models
Payers have complex systems, flexibility helps you stand out. You can propose:
- Per-member-per-month (PMPM) fee model — predictable revenue.
- Outcome-based model — tied to clinical or cost benchmarks.
- Shared-savings agreement — both sides benefit from reduced claims.
Make your offer scalable and easy to integrate within their existing network structure.
Step 4: Demonstrate Compliance and Integration Readiness
Compliance is a top priority for payers. Show that your RPM program meets all HIPAA, CMS, and interoperability standards. Key documentation to present:
- HIPAA compliance certificates.
- Business Associate Agreements (BAA) templates.
- FHIR and HL7 integration support for EHR/claims data.
Emphasize how your system securely shares patient readings with care teams.
Step 5: Engage Through Pilot Programs
Payers rarely commit to full-scale deployment immediately. Offer a 3- to 6-month pilot with measurable KPIs. Track and report:
- Number of enrolled members.
- Compliance rate and daily reading frequency.
- Outcome improvements (BP reduction, medication adherence).
Once the pilot proves value, move toward a network-wide rollout.
Step 6: Provide Transparent Reporting and Support
Regular communication is the foundation of payer relationships. Offer real-time dashboards for claims, compliance, and patient metrics. Schedule quarterly business reviews to discuss:
- ROI and clinical outcomes.
- Areas for scaling or additional conditions.
- New reimbursement opportunities (like upcoming CPT 99XX4 and 99XX5 codes).
Key Takeaway
Payers look for proof, not potential. The more data, compliance readiness, and reporting transparency you offer, the stronger your RPM partnership proposal will be.
How CandiHealth Simplifies RPM Partnerships
Building partnerships with clinics or payers for Remote Patient Monitoring can be challenging, from compliance and billing complexities to device logistics and patient engagement.
CandiHealth eliminates these hurdles through a ready-to-launch RPM solution that’s designed for seamless integration, transparent pricing, and measurable outcomes.
Here’s how CandiHealth makes RPM partnerships simple, scalable, and sustainable.
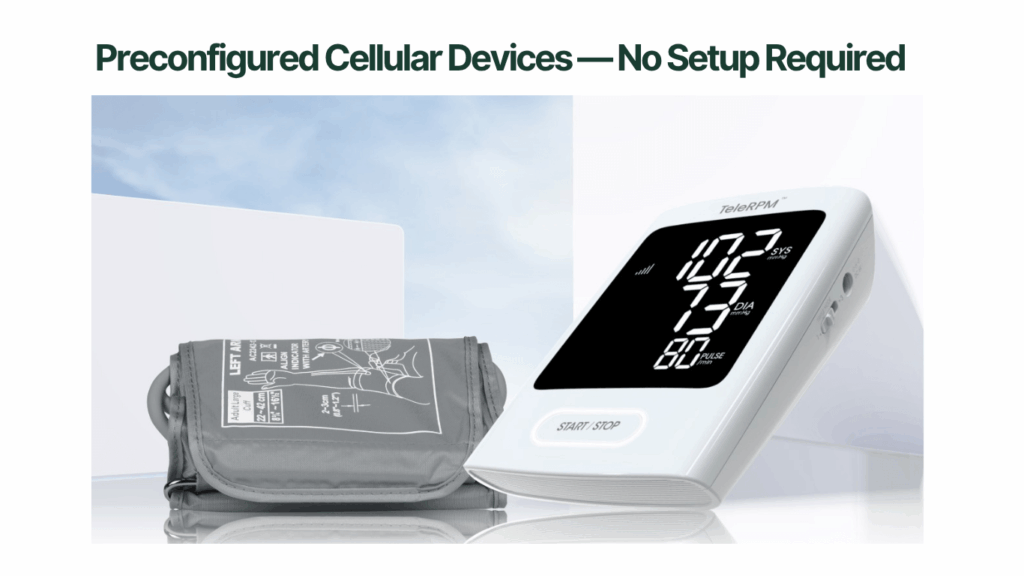
1. Preconfigured Cellular Devices — No Setup Required
CandiHealth provides cellular-connected blood pressure monitors that work out of the box — no Wi-Fi or app downloads required. This is a game changer for clinics and payers:
- Patients just unbox, use, and start transmitting readings automatically.
- Clinics avoid complex tech support calls.
- Payers receive reliable data for compliance and reporting.
2. Flat-Fee Model — Transparent Costs for Everyone
Instead of unpredictable revenue-sharing or per-reading models, CandiHealth offers a flat-fee pricing structure.
- Clinics know exactly what they’ll pay per enrolled patient.
- Payers can forecast costs confidently without hidden platform fees.
- Vendors gain predictable margins to scale operations.
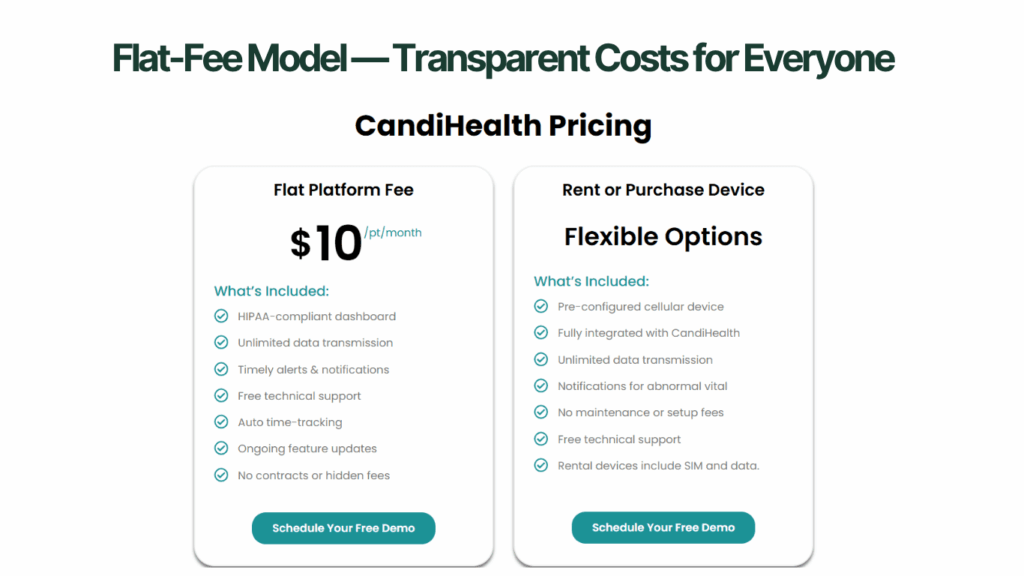
This model allows smaller clinics and regional payers to start RPM programs without worrying about billing complexity or variable device costs.
3. Built-in Compliance and CMS-Ready Documentation
CandiHealth ensures every partner stays compliant from day one. The platform includes auto-logged CPT time tracking (for 99453–99458) and HIPAA-secure dashboards with audit trails. This means clinics and payers don’t need separate compliance tools or consultants — everything is built in.
If you’re a clinic or payer ready to simplify your RPM journey, CandiHealth is built for you.
- No complex integrations.
- No unpredictable fees.
- Just results — better outcomes, higher compliance, and measurable ROI.
Book a Partnership Call with CandiHealth and see how easily you can launch your RPM program.
Frequently Asked Questions (FAQs)
Q1. Who can order and bill for Remote Patient Monitoring (RPM) services?
Only licensed healthcare providers, such as physicians, nurse practitioners, and physician assistants, can order and bill for RPM under Medicare CPT codes 99453–99458. Clinical staff can help collect data, but billing must be submitted under the supervising provider’s NPI.
Q2. What is the RPM program in healthcare?
Remote Patient Monitoring (RPM) allows clinicians to track patients’ health data outside the clinic using connected medical devices. Common metrics include blood pressure, glucose, and weight. RPM helps detect early signs of worsening conditions and reduces hospital visits, improving both care quality and patient satisfaction.
Q3. How to start an RPM business?
Starting an RPM business begins with:
- Choosing an FDA-cleared device and HIPAA-compliant platform.
- Understanding Medicare billing rules and CPT codes.
- Partnering with clinics that treat chronic patients.
- Setting up patient onboarding, monitoring, and documentation systems.
Using an end-to-end solution like CandiHealth can simplify this process with preconfigured cellular devices and flat-fee pricing.
Q4. What is the RPM system in healthcare?
An RPM system combines medical devices, cloud software, and reporting tools that transmit patient vitals in real time. It enables clinicians to review readings, track progress, and intervene early. For example, CandiHealth’s RPM system automatically sends blood pressure readings from a cellular device to a secure provider dashboard.